Find out more about BAPO’s mentorship programme, which is available to members at any stage of their their career (including learners) to enable them to gain personalised guidance on a range of topics.
Learning UK Working Group. Principles for Continuing Professional Development and Lifelong Learning in Health and Social Care.”
CPD and lifelong learning are necessary for the development of everyone who works in health and social care. This document sets out princiles that you can apply to help you manage and take ownership of your own CPD to meet the HCPC requirements that apply once you are registered.

BAPO offers regular webinars and short courses. Check out the latest offerings and how to register for them via these links. These events are open to members and non-members.
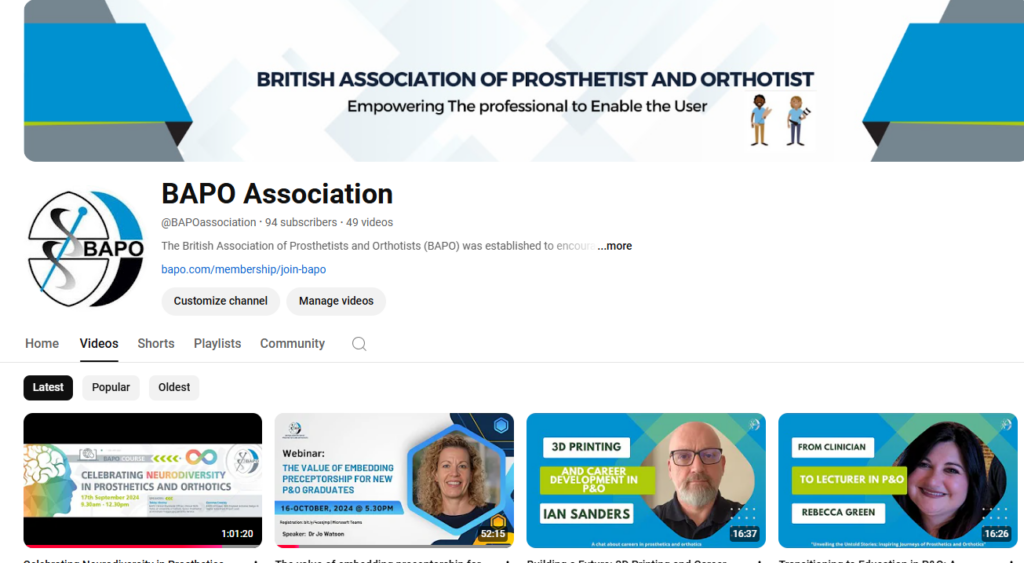
The BAPO YouTube channels contains a range of video resources spanning subject areas such as BAPO Learning, dementia awareness, interviews with members of the P&O workforce, and BAPO event highlights.
BAPO runs regular TeaTime Talks and other virtual events for members. You can find out about forthcoming events and (if you are a member) register for then here.
These member-only video resources cover topics such as clinical note-keeping and consent, what the Health and Care Professions Council (HCPC) is and how to register with it when you qualify, and continuous professional development.
This member-only resource provides guidance and advice about preparing poster presentations for all kinds of conferences. These are essential skills to develop as part of the research pillar of practice. And they’re potentially very useful for any of your assessments that involve a poster presentation.

This step-by-step guide will help you develop your skills and confidence in literature searching in research databases. These are essential skills to develop as part of the research pillar of practice. And they’ll help a great deal with your current studies.
BAPO runs a number of annual regional conferences around the UK. Students and apprentices are welcome to join in. Find out more here.

BAPO makes a number of annual awards to members of the professional community, including Student of the Year. Check out details here.
Responding directly to a need identified by learners, this comprehensive resource guides you through the different elements you will need to consider to ensure that you are well-prepared to apply for jobs and participate in job interviews in prosthetics and orthotics.